2025 Behavioral Health Plan Transition
Your wellbeing is a priority. The University is committed to cultivating a campus environment where all faculty, staff, and students can thrive. Part of this commitment includes providing access to quality behavioral and mental health care through the University’s employee benefit plans.
Bottom Line, Up Front:
- Wake Forest will continue to offer behavioral health coverage to benefits-eligible faculty and staff who are enrolled in the University’s medical plan in 2025.
- Wake Forest will transition from Carolina Behavioral Health Alliance (CBHA) to Aetna as the third-party administrator for behavioral health coverage beginning January 1, 2025.
- Instructions for determining whether your current provider is in-network with Aetna and finding a new provider, if necessary, are below.
- Additional Behavioral Health coverage changes are not anticipated for the 2025 plan year, but coverage details and cost will not be finalized until shortly before the open enrollment period (October 7-18, 2024).
Navigation
- Preparing for the Transition
- Joining the Aetna network
- Frequently Asked Questions
- Behavioral Health Resources
Questions? We invite you to share your questions, feedback, and concerns about this transition.
Preparing for the Transition
The transition from CBHA to Aetna will not occur until January 1, 2025. If you take advantage of the University’s behavioral health plan, we encourage you to proactively determine whether your current behavioral health provider is in-network and, if necessary, find a new in-network provider during this 8-month transition.
- Step 1: Confirm your Aetna network
- Step 2: Check to see if your provider is in-network with Aetna
- Step 3: Find a new in-network provider, if necessary
Aetna Customer Service
Aetna is available to help WFU members verify whether their current behavioral health provider is in-network and identify a new in-network provider if needed.
- Email wfu@aetna.com
- Call 855.586.6961
These instructions are also outlined in this printer-friendly Transition Toolkit.
Step 1: Confirm your Aetna network
Before you begin, determine which Aetna network you are enrolled by completing the instructions below:
- Log into Workday
- Click the Menu dropdown in the top left corner
- Select the Benefits and Pay app
- Click the Benefits dropdown (shield icon) in the left sidebar
- Select the Benefit Elections link
- Your medical plan network will be listed in the Benefit Plan column as either “Aetna Whole Health Choice POS II” or “Aetna Whole Health”
Step 2: Check to see if your provider is in-network with Aetna
Once you know which Aetna network you are enrolled in (Step 1), you can search the Aetna provider database to see if your behavioral health provider is already in-network by following the instructions below:
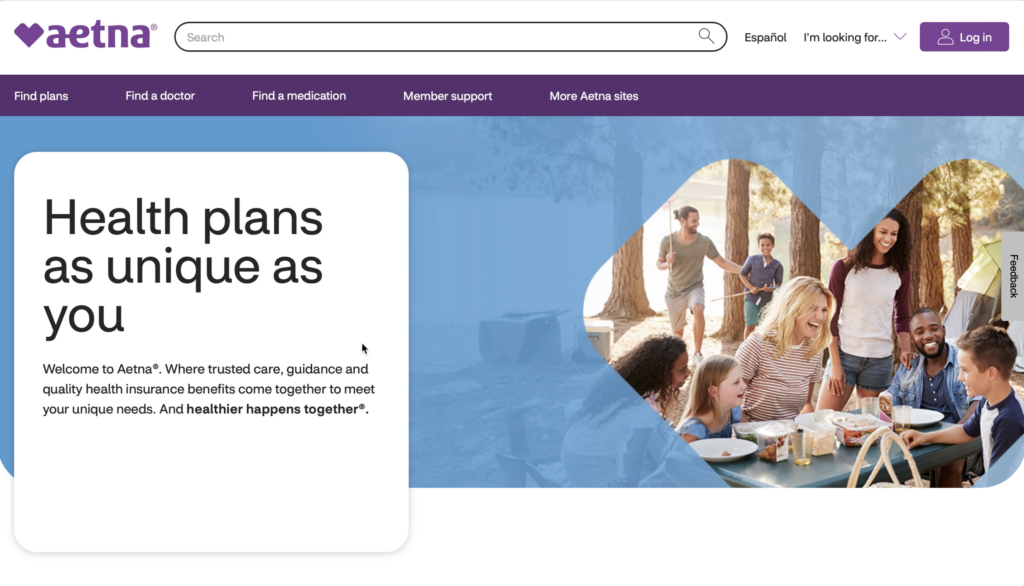
- Visit aetna.com
- Click Find a Doctor at the top of the page
- Click Plan from an Employer in the “Don’t have a member account?” box
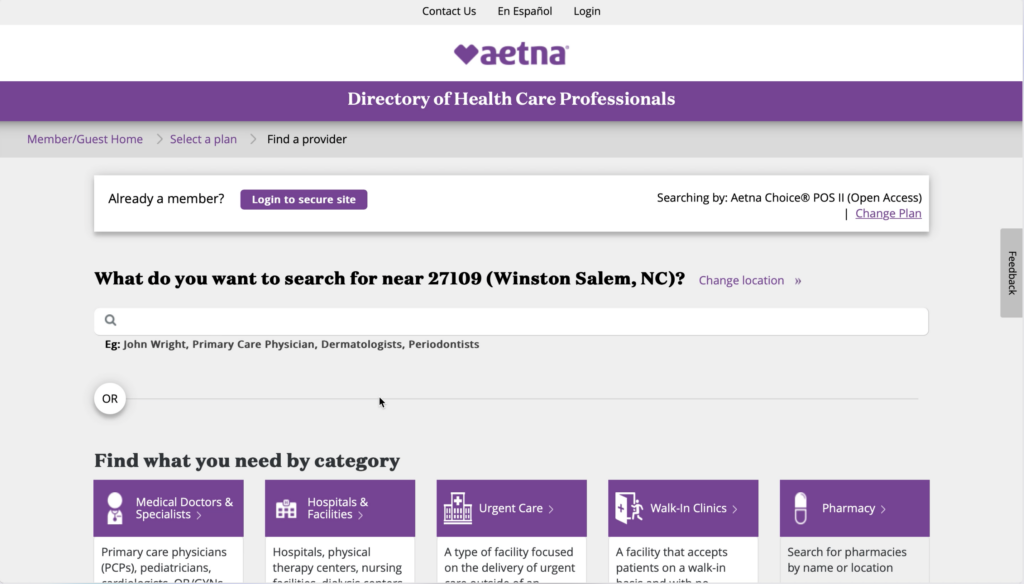
- Enter a zip code in the “Continue as guest box” and adjust search miles, if desired, and click the Search button
- Click (NC and SC) Aetna Whole Health – Atrium Health) under “Aetna Whole Health Plans” or Aetna Choice POS II (Open Access) under “Aetna Open Access Plans” in the “Select a Plan” box – your network selection should be based on what is listed in Workday in Step 1.
- Click the Continue button
- Enter the name of the provider or practice in the Search Bar and click on the provider name to confirm they are in-network
Important: If your provider does not appear in the search, reach out to Aetna directly at wfu@aetna.com or 855.586.6961 to confirm whether your current provider is in-network with Aetna. You may also contact your provider directly to inquire.
Step 3: Find a new in-network provider, if necessary
If you find that your provider is out-of-network in Step 2, first follow instructions 1-6 outlined above and then complete the instructions below to identity new in-network providers:
- You may find a provider by either entering provider specialty (i.e. Psychologist, Psychiatrist, etc.) into the Search Bar or scroll down to the Find what you need by category section
- Click the Mental Health box
- Click the Mental Health Professionals box
- Click on the type of support that is needed (i.e. Anxiety and Stress Management Counseling, Autism Spectrum Disorder, Cognitive Behavioral Therapy, Depression, Eating Disorder, LGBTQIA, Post-Traumatic Stress Disorder, etc.)
- Review the list of in-network providers
Joining the Aetna Network
Aetna is proactively contacting out-of-network providers to invite them to join the Aetna network, however the provider ultimately makes that decision. If your current behavioral health provider is out-of-network, you may invite them to join the Aetna network with this language:
“Wake Forest will be transitioning from CBHA to Aetna in 2025. I value our patient-provider relationship and hope you will consider joining Aetna’s network. You can learn more about joining at https://www.aetna.com/health-care-professionals/join-the-aetna-network.html.”
Share Your Concerns
We invite you to share your questions, feedback, and concerns about this transition with us.
Frequently Asked Questions
While there are a significant number of factors that inform a third-party administrator transition, the following three were among the most important for this particular change: (1) we are at a moment of limited disruption, (2) we are committed to compliance, and (3) we need to offset rising health care costs. Additional information about how the University came to this decision is available in this Fact Sheet.
No. Wake Forest will continue to provide access to behavioral health coverage to benefits-eligible faculty and staff who are enrolled in the University’s medical plan in 2025.
The University anticipates behavioral health coverage to significantly remain the same for the 2025 plan year, however any potential changes to coverage, premiums, copays, deductibles, and out-of-pocket maximums will be finalized in September, prior to Open Enrollment in October.
Prescriptions are covered under the University’s Pharmacy Plan, which reviews the formulary once a quarter and communicates any prescription changes to impacted members.
The University will continue to evaluate claims data to inform any other possible benefit changes for 2025. Any changes to coverage, premiums, copays, deductibles, and out-of-pocket maximums will be finalized in September, prior to Open Enrollment in October.
You may use any behavioral health provider of your choosing. If your provider is out-of-network with Aetna, you will be responsible for a percentage of the cost of services after meeting your deductible. The cost of copayments and deductibles depend on your enrolled plan (High Plan or Low Plan) and which tier the provider is in.
Yes, you may change providers at any time. However, if you change providers before January 1, 2025, it is important to ensure this provider is in-network with both CBHA and Aetna.
Aetna will proactively reach out to out-of-network providers and invite them to join the Aetna network, however the provider ultimately makes that decision. You are invited to encourage your current provider to join the Aetna network.
Decisions regarding the University’s benefits suite are made in coordination with the University leadership and Human Resources. The Fringe Benefits Advisory Committee provides advice on potential recommendations and decisions by sharing feedback from their constituencies.
The University evaluates all our third-party benefits administrators on a regular basis. The decision to transition away from CBHA to Aetna was made in March 2024, with the Fringe Benefits Advisory Committee being informed on March 27. CBHA and Aetna were informed about the decision on April 8 and 10, respectively.
The University always wants input from faculty and staff. However, this decision has already been approved by senior leadership, and CBHA and Aetna have already been informed of the transition.
Colleagues may submit questions, concerns, and feedback using this Google Form.
Ongoing and New Behavioral Health Resources
Employee Assistance Program
Confidential professional assessment, referral, and follow-up services for a variety of behavioral health needs. Call 336.716.5493 for an appointment.
New York Life EAP
Confidential consultation and referral services offered by telephone 24/7. Call 800.344.9752.

Teladoc Health
Effective January 1, 2025, the current Teladoc Health program will include behavioral health support 24/7 for members age 13 years and older.
Wake Forest University Human Resources
P.O. Box 7424, Winston-Salem, NC 27109
askHR@wfu.edu | P 336.758.4700 | F 336.758.6127
